Cognitive Decline Due to Aging Can Be Reversed in Mice – Here’s What The New Study Means For Humans
 By Richard Faragher, University of Brighton
By Richard Faragher, University of Brighton
The ageing global population is the greatest challenge faced by 21st-century healthcare systems. Even COVID-19 is, in a sense, a disease of ageing. The risk of death from the virus roughly doubles for every nine years of life, a pattern that is almost identical to a host of other illnesses. But why are old people vulnerable to so many different things?
It turns out that a major hallmark of the ageing process in many mammals is inflammation. By that, I don’t mean intense local response we typically associate with an infected wound, but a low grade, grinding, inflammatory background noise that grows louder the longer we live. This “inflammaging” has been shown to contribute to the development of atherosclerosis (the buildup of fat in arteries), diabetes, high blood pressure , frailty, cancer and cognitive decline.
Now a new study published in Nature reveals that microglia – a type of white blood cells found in the brain – are extremely vulnerable to changes in the levels of a major inflammatory molecule called prostaglandin E2(PGE2). The team found that exposure to this molecule badly affected the ability of microglia and related cells to generate energy and carry out normal cellular processes.
[do_widget id=text-16]
Fortunately, the researchers found that these effects occurred only because of PGE2’s interaction with one specific receptor on the microglia. By disrupting it they were able normalise cellular energy production and reduce brain inflammation. The result was improved cognition in aged mice. This offers hope that the cognitive impairment associated with growing older is a transient state we can potentially fix, rather than the inevitable consequence of ageing of the brain.
Reversing cognitive decline
Levels of PGE2 increase as mammals age for a variety of reasons – one of which is probably the increasing number of cells in different tissues entering a state termed cellular senescence. This means they become dysfunctional and can cause damage to tissue by releasing PGE2 and other inflammatory molecules.
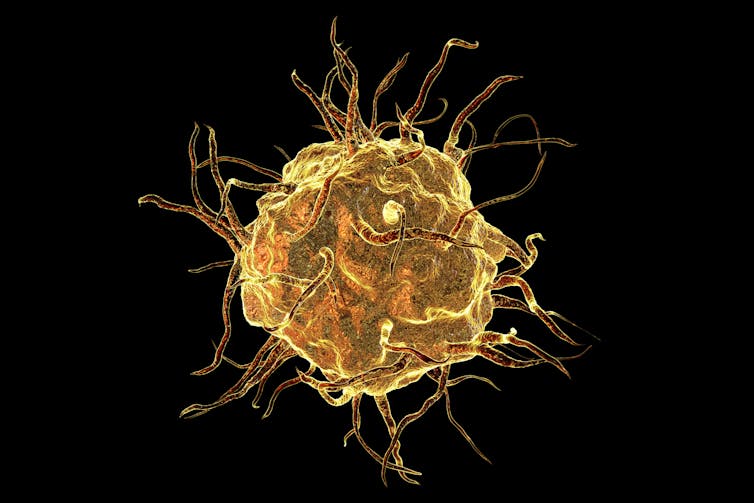
Macrophage cell. Kateryna Kon/Shutterstock
But the researchers also found that macrophages – another type of white blood cells related to microglia – from people over the age of 65 made significantly more PGE2 than those from young people. Intriguingly, exposing these white blood cells to PGE2 suppressed the ability of their mitochondria – the nearest thing a cell has to batteries – to function. This meant that the entire pattern of energy generation and cellular behaviour was disrupted.
Although PGE2 exerts its effects on cells through a range of receptors, the team were able to narrow down the effect to interaction with just one type (the “EP2 receptor” on the macrophages). They showed this by treating white blood cells, grown in the lab, with drugs that either turned this receptor on or off. When the receptor was turned on, cells acted as if they had been exposed to PGE2. But when they were treated with the drugs that turned it off, they recovered. That’s all fine, but it was done in a petri dish. What would happen in an intact body?
FREE PDF: 10 Best Books To Survive Food Shortages & Famines
The researchers then carried out one of the cleanest experiments it is possible to perform in biology and one of the best reasons for working on mice. They took genetically modified animals in which the EP2 receptor had been removed and allowed them to grow old. They then tested their learning and memory by looking at their ability to navigate mazes (something of a cliche for researchers) and their behaviour in an “object location test”. This test is a bit like someone secretly entering your house, swapping your ornaments around on the mantelpiece and then sneaking out again. The better the memory, the longer the subject will spend looking suspiciously at the new arrangement, wondering why it has changed.
It turned out that the old genetically modified mice learned and remembered just as well as their young counterparts. These effects could be duplicated in normal old mice by giving them one of the drugs that could turn the EP2 receptor off for one month. So it seems possible that inhibiting the interaction of PGE2 with this particular receptor may represent a new approach to treating late-life cognitive disorders.
There is a long way to go before we are in a position to start using these compounds in humans – even though the prostaglandin systems are very similar. But this study has shed light on a fascinating set of observations linking diet and cognition.
It has been known for some years that eating blueberries and other fruit and vegetables, such as strawberries and spinach, improves cognition in rodents and older people. These foods are rich in molecules such as resveratrol, fisetin and in quercetin, which have been shown either to kill or rescue senescent cells.
There is also evidence that they block PGE2 at the cellular level, providing another route by which these compounds may exert their beneficial effects. Until something better comes along, this is one more piece of evidence that a bowl of fruit won’t do you any harm. Though it’s probably wise to go easy on the cream.![]()
Richard Faragher, Professor of Biogerontology, University of Brighton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Top image: Memory declines with age. Robert Kneschke/Shutterstock


