Physician and Medical Journal Editor: Healthy People Should Not Wear Face Masks
 Healthy People Should Not Wear Face Masks
Healthy People Should Not Wear Face Masks
by Jim Meehan, MD
MeehanMD.com.
Via Health Impact News:
During the COVID-19 pandemic, public health experts began telling us to follow a number of disease mitigation strategies that sounded reasonably scientific, but actually had little or no support in the scientific literature. Community wearing of masks was one of the more dangerous recommendations from our confused public health experts.
[do_widget id=text-16]
The Pandemic of Bad Science and Public Health Misinformation on Community Wearing of Masks
Renowned neurosurgeon, Russell Blaylock, MD had this to say about the science of masks:
As for the scientific support for the use of face masks, a recent careful examination of the literature, in which 17 of the best studies were analyzed, concluded that, “None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”[R] Keep in mind, no studies have been done to demonstrate that either a cloth mask or the N95 mask has any effect on transmission of the COVID-19 virus. Any recommendations, therefore, have to be based on studies of influenza virus transmission. The fact is, there is no conclusive evidence of their efficiency in controlling flu virus transmission. – Russell Blaylock, MD
You can read Dr. Blaylock’s brilliant discussion of this matter at the end of this paper or at this link:
Blaylock: Face Masks Pose Serious Risks to the Healthy
Quarantining Healthy People – A Failed Experiment
We were told that everyone, even the healthy, should quarantine at home. All were told to “shelter-in-place,” isolate ourselves, hide alone, indoors, until the danger of the virus passed, despite the large body of scientific evidence that shows our immune systems thrive on diversity of exposures, sunlight, time in nature, and in loving company of others.
Furthermore, it seemed that the public health experts were ignoring the very real harms that result from shutting down the economy, putting tens of millions of workers out of work, and the shadow pandemic of suicides, drug abuse, overdoses, and other harms that follow massive economic downturns. [R][R]
Historically and by definition, quarantines had always been about sequestering the sick. Never before had anyone beat a virus by quarantining the healthy. We were not told that quarantining healthy people was a first-of-its kind experiment. And the experiment failed. More on this topic later.
Community Wearing of Masks is a Bad Recommendation
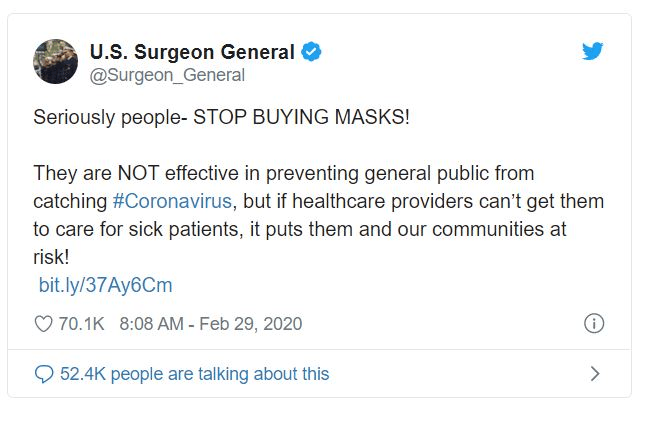
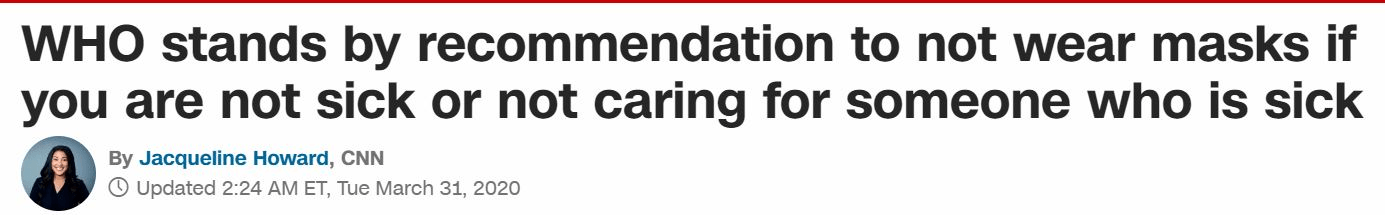
We were frequently confused by the mixed messages coming from public health agencies. Early in the pandemic Dr. Fauci, the U.S. Surgeon General, and the WHO all told the public, in no uncertain terms, not to wear masks. Then, over the course of the next several weeks and months, the CDC twice changed their recommendations, as did the WHO, and the recommendations always contradicted each other!
The CDC made the mistake of telling us cloth masks worked, and they even provided directions on their website for making homemade cloth masks.
To clear up the confusion, I will show that the scientific evidence not only does not support the community wearing of face masks, but the evidence shows that healthy people wearing face masks pose serious health risks to wearers.
Hiding our faces behind masks and isolating in our homes is not the solution, at least not for most people with healthy immune systems. Supporting the health of your immune system, confidently confronting all pathogens, and allowing herd immunity to develop and protect the vulnerable populations should be the goal.
What’s happening in the world today, including the misinformation surrounding community mask wearing, is about political agendas, symbolism, fear, and dividing and isolating the people. It has nothing to do with science.
Medical Masks are Bad for Health
As a physician and former medical journal editor, I’ve carefully read the scientific literature regarding the use of face masks to mitigate viral transmission. I believe the public health experts have community wearing of masks all wrong. What follows are the key issues that should inform the public against wearing medical face masks during the CoVID-19 pandemic, as well as all future respiratory disease pandemics.
Face masks decrease oxygen, increase carbon dioxide, and alter breathing in ways that increase susceptibility and severity of CoVID-19
Mask wearers frequently report symptoms of difficulty breathing, shortness of breath, headache, lightheadedness, dizziness, anxiety, brain fog, difficulty concentrating, and other subjective symptoms while wearing medical masks. As a surgeon, I have worn masks for prolonged periods of time in thousands of surgeries and can assure you these symptoms do occur when surgical masks are worn for extended periods of time. The longer a surgical mask is worn, the more saturated with moisture it becomes, and the more significantly it inhibits the inflow of oxygen and outflow of carbon dioxide.
In fact, clinical research shows that medical masks lower blood oxygen levels[R] and raise carbon dioxide blood levels.[R] The deviations in oxygen and carbon dioxide may not reach the clinical criteria for hypoxia (low blood oxygen), hypoxemia (low tissue oxygen), or hypercapnia (elevated blood carbon dioxide), but they can deviate enough to cause even healthy individuals to become symptomatic, as occurred with the surgeons studied and published in this report:
Preliminary Report on Surgical Mask Induced Deoxygenation During Major Surgery
At the same time masks inhibit oxygen intake, they trap the carbon dioxide rich breath in the mouth/mask inter-space. Thus, a fraction of carbon dioxide previously exhaled is inhaled at each respiratory cycle.
Masks force you to re-breathe a portion of your own breath, including all the stuff (infectious viral particles) the lungs were trying to remove from the body (more on this later).
As medical masks lower oxygen and raise carbon dioxide in the blood, the brain senses the changes and the risk they pose to the maintenance of normal physiology. Thus, the brain goes to work to bring things back in order. To obtain more oxygen and remove more carbon dioxide, the brain tells the lungs to increase the rate (frequency) and depth of breaths.[R] Unfortunately, struggle as they may, your brain and lungs can not fully compensate for the negative effects of the mask. Some may even suffer the symptoms of carbon dioxide toxicity.
For people with diseases of the lungs, especially chronic obstructive pulmonary disease (COPD), face masks are intolerable to wear as they worsen breathlessness.[R]
In the case of respiratory pathogens, the negative effects of masks and the respiratory changes they induce could increase susceptibility and transmission of CoVID-19, as well as other respiratory pathogens.
Viral particles move through face masks with relative ease. Studies show that about 44% of viral particles pass through surgical masks, 97% pass through cloth masks, and about 5% through N95 masks. Increasing tidal volume (depth of breaths) results in literally sucking more air, more forcefully through and around the mask. Any SARS CoV-2 particles on, in, or around the mask are more forcefully suctioned into the mouth and lungs as a result of the compensatory increases in tidal volume.
The changes in respiratory rate and depth may also increase the severity of CoVID-19 as the increased tidal volume delivers the viral particles deeper into the lungs.
These changes may worsen the community transmission of CoVID-19 when infected people wearing masks exhale air more heavily contaminated with viral particles from the lungs.
These effects are amplified if face masks are contaminated with the viruses, bacteria, or fungi that find their way or opportunistically grow in the warm, moist environment that medical masks quickly become.
Despite the scientific evidence to the contrary, public health experts claim that medical masks do not cause clinically significant hypoxia (low oxygen) and hypercapnia (high CO2). I would like to ask those experts to explain the growing number of cases in which medical masks worn during exercise have resulted in lung injuries and heart attacks:
Two Chinese boys drop dead during PE lessons while wearing face masks amid concerns over students’ fitness following three months of school closure [R][R]
Jogger’s lung collapses after he ran for 2.5 miles while wearing a face mask [R]
If medical masks were perfectly safe and effective, then why would healthy boys suffer heart attacks or a 26 year old man collapse his lung while wearing masks and running?! In my opinion, these are tragic examples of the risks of wearing medical masks. And we are only getting started.
SARS CoV-2 becomes more dangerous when blood oxygen levels decline
Low blood levels of oxygen is a critical issue in the pathogenicity of CoVID-19. The virus’ ability to infect cells is markedly enhanced by oxygen desaturation, which we know occurs when wearing a surgical mask.[R]
One of the features that make SARS CoV-2 uniquely infectious is the “furin cleavage” sequence in the virus that activates increased ACE2 receptor attack and cellular invasion in low oxygen environments.[R]
The furin cleavage site of SARS CoV-2 increases cellular invasion, especially during hypoxia (low blood oxygen levels)[R]
The furin cleavage site found in SARS CoV-2 is the likely result of the bio-engineering “gain of function” (increasing the virulence of a pathogen) research conducted at the Wuhan Institute of Virology. This unethical, dangerous, and illegal-in-most-countries research is alleged to have been funded by Dr. Anthony Fauci (with $7.4 million taxpayer dollars) and Bill Gates.
Furin cleavage sites are found in some of the most pathogenic forms of influenza. The furin cleavage domain in SARS CoV-2 is cleaved by furin on the target cell.
Furin is an ubiquitous protease in humans. It is found in a wide variety of tissues in the human body: heart, brain, kidney, etc. It is expressed in significant concentrations in human lung cells, the common target of SARS CoV-2. When the virus encounters a lung cell expressing (both an ACE2 receptor and furin), the furin cleaves the furin cleavage site on SARS CoV-2, activates the virus’ surface S (spike) protein, and enables the virus to more effectively bind the ACE2 receptors and more efficiently invade the cell.[R]
Remember how medical face masks decrease blood oxygen levels? Well, now you need to know that SARS CoV-2’s ability to invade and infect our cells is greatly enhanced under conditions of low oxygen.[R]
Therefore, wearing a medical mask may increase the severity of CoVID-19. If that does not motivate you to ditch your mask, there are more reasons to come.
Some of the most pathogenic forms of influenza and HIV are armed with similar furin cleavage sites. However, furin cleavage sites are not present in other beta coronaviruses. The furin cleavage site is NOT present in SARS CoV-1, MERS, or the other “bat coronaviruses” postulated to be the progenitors of SARS CoV-2.
It is worth repeating: SARS-CoV, which is closely related to the newest SARS-CoV-2 strain, does not bear the furin cleavage site. So how did SARS CoV-2 gain the furin cleavage function?
Dr. Fauci built his career on HIV research, HIV vaccine failures, and unethical “gain of function” research. He undoubtedly knows a lot about furin cleavage sites and the suspicious origins of SARS CoV-2. Perhaps Congress should ask him…under oath…preferably with an indictment.
The question we should all be asking is how did the genetic sequence that codes for this serious gain of function that increases the potential for the virus to successfully infiltrate the host find its way into SARS-CoV-2? That’s the trillion dollar question; it demands a real answer.
Medical masks trap exhaled viral particles in the mouth/mask interspace, increase viral load, and increase the severity of disease.
Face masks trap exhaled viral particles in the mouth/mask inter-space.[R] The trapped viral particles are prevented from removal from the airways. The mask wearer is thus forced to re-breathe the viral particles, increasing infectious viral particles in the airways and lungs. In this way, medical masks cause self-inoculation, increase viral load, and increase the severity of disease.
Asymptomatic or mild cases of CoVID-19 become more severe when an infected individual is masked, oxygen lowers, viral load increases from particle re-breathing, and the disease overwhelms the innate immune system.
- The main purpose of the innate immune response is to immediately prevent the spread and movement of foreign pathogens throughout the body.[R]
- The innate immune system plays a crucial role in destroying the virus, preventing infection, or decreasing the viral load to decrease the severity of infection.
- The innate immunity’s effectiveness is highly dependent on the viral load. If face masks increase viral particle re-breathing at the same time they create a humid habitat where SARS-CoV-2 remains actively infectious, the mask increases the viral load and can overwhelm the innate immune system.
This trapping, re-breathing, and increasing pathogen load delivered to the lungs becomes dramatically more dangerous when the medical mask becomes contaminated with the opportunistic viruses, bacteria, and fungi that can grow in the warm, moist environment of the mask.
“By wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, enter the olfactory nerves and travel into the brain.” – Russell Blaylock, MD
Masks are unnecessary when asymptomatic spreading of SARS CoV-2 is “very rare”
Much of the recommendation for community wearing of masks was based on the belief that asymptomatic carriers of SARS CoV-2 were responsible for the transmission and spread of CoVID-19. There was no real scientific evidence for this belief. However, antibody testing began demonstrating larger numbers of people with antibodies to the virus than anyone imagined. Therefore, the belief was that these people must represent asymptomatic carriers that were spreading the disease.
Contact tracing has determined that asymptomatic cases are not causing secondary transmission:
Asymptomatic spread of coronavirus is “very rare,” WHO says
“We have a number of reports from countries who are doing very detailed contact tracing,” she [Dr. Maria Van Kerkhove, head of WHO’s emerging diseases and zoonosis unit], said. “They’re following asymptomatic cases. They’re following contacts. And they’re not finding secondary transmission onward. It’s very rare.”
More from the article:
Coronavirus patients without symptoms aren’t driving the spread of the virus, World Health Organization officials said Monday, casting doubt on concerns by some researchers that the disease could be difficult to contain due to asymptomatic infections.
Some people, particularly young and otherwise healthy individuals, who are infected by the coronavirus never develop symptoms or only develop mild symptoms. Others might not develop symptoms until days after they were actually infected.
Preliminary evidence from the earliest outbreaks indicated that the virus could spread from person-to-person contact, even if the carrier didn’t have symptoms. But WHO officials now say that while asymptomatic spread can occur, it is not the main way it’s being transmitted.
“From the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” Dr. Maria Van Kerkhove, head of WHO’s emerging diseases and zoonosis unit, said at a news briefing from the United Nations agency’s Geneva headquarters. “It’s very rare.”
The fact that asymptomatic carriers are not a major driver of the disease tells us that masks are unnecessary.
The Evidence for Aerosol Transmission is Weak
The likelihood of airborne transmission—especially compared with other routes, such as droplets or surfaces—remains unclear. Most researchers still think the new coronavirus is primarily spread via droplets and touching infected people or surfaces. So diligent hand washing and social distancing are still the most important measures people can take to avoid infection.”[Scientific American, 5/12/2020]
Wearing a face mask may give a false sense of security
- Wearing a face mask may give a false sense of security.
- People adopt a reduction in compliance with other infection control measures, including social distancing and hands washing.[R]
Inappropriate use of face masks:
- People must not touch their masks, must change their single-use masks frequently or wash them regularly, dispose them correctly and adopt other management measures, otherwise their risks and those of others may increase.[R][R]
Wearing a face mask makes the exhaled air go into the eyes.
- This generates an uncomfortable feeling and an impulse to touch your eyes. If your hands are contaminated and you touch or rub your eyes, you are infecting yourself.[R]
Masks compromise communications and reduce social distancing
- The quality and volume of speech between two people wearing masks is considerably compromised, so they may unconsciously move closer to improve communications.
- This increases the likelihood of becoming exposed to respiratory droplets containing infectious viral particles.
Contact tracing studies show that asymptomatic carrier transmission is very rare.
- Asymptomatic carriers are not a major driver of the disease.[R]
- Therefore, masks are unnecessary.
- Furthermore, social distancing is unnecessary.
Face masks and stay at home orders prevent the development of herd immunity.
- Only herd immunity can prevent pandemics.
- Only herd immunity will protect the vulnerable members of society.
Lack of Scientific Evidence for Community Wearing of Face Masks
There is no reasonable scientific evidence to support healthy people wearing masks. Russell Blaylock, MD had this to say about the science of masks:
As for the scientific support for the use of face mask, a recent careful examination of the literature, in which 17 of the best studies were analyzed, concluded that,“None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”[R] Keep in mind, no studies have been done to demonstrate that either a cloth mask or the N95 mask has any effect on transmission of the COVID-19 virus. Any recommendations, therefore, have to be based on studies of influenza virus transmission. The fact is, there is no conclusive evidence of their efficiency in controlling flu virus transmission.[R]
Here’s what a group of physicians wrote regarding Universal Masking in Hospitals in the CoVID-19 Era in the New England Journal of Medicine:
We know that wearing a mask outside healthcare facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to CoVID-19 as face-to-face contact within 6 feet with a patient with symptomatic CoVID-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching CoVID-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.
The clinical research on this topic is clear: even when handled and worn properly, which is definitely NOT happening in the public spaces, wearing a mask in public offers little or no protection from infection. However, when masks are handled and worn improperly, they are a personal and public health disaster.
The “Hamster Study” is an example of weak science used to support bad recommendations
Here’s an example of one of the experimental studies used by some public health authorities to support wearing masks in the community:
Wearing a mask can significantly reduce coronavirus transmission, study on hamsters claims
Does this study of “masking” hamster cages sound like the kind of solid scientific evidence that supports recommendations or mandates for everyone to wear masks during the CoVID-19 pandemic? No. The hamsters were not forced to wear tiny hamster surgical masks, their cages were covered with a barrier made of mask-like material. The experiment was more about walls or barriers than it was masks.
The experiment did not create the same conditions experienced by masked humans. Placing a cloth barrier on hamster cages is nothing like masking the mouth and nose of humans. The way this experiment was set up, inhalations were unimpeded, therefore, arterial oxygen levels would not be expected to lower. Likewise, exhalations were not trapped in a way that would force the hamsters to suffer re-breathing their own carbon-dioxide or subject them to the dangers of re-inhaling the infectious viral particles released with each exhalation.
This study does not provide support for the recommendation for masking all members of the public to reduce transmission of SARS CoV-2. Those citing this study to support wearing masks in the community are inappropriately extrapolating and conflating the experiment’s findings to contrive a conclusion the experimental methodology does not allow.
Some studies even question the efficacy of surgical masks in the operating room
Surgical face masks in modern operating rooms—a costly and unnecessary ritual?
Following the commissioning of a new suite of operating rooms, air movement studies showed a flow of air away from the operating table towards the periphery of the room. Oral microbial flora dispersed by unmasked male and female volunteers standing one meter from the table failed to contaminate exposed settle plates placed on the table. The wearing of face masks by non-scrubbed staff working in an operating room with forced ventilation seems to be unnecessary.
Public Health Experts Are Confused and Contradictory on Masks
Since the first days of the pandemic, Fauci, Birx, the CDC, and the WHO have been confusing the public as they flipped, flopped, and contradicted each other on the community wearing of medical masks. We should expect more than confusing, contradictory, unevidenced advice from our public health experts.[R][R] Their lack of evidence and clarity was subverted to the belief that any level of protection was better than none. However, no one seemed to be fully considering the downsides of masks as I have presented them above.
Early in the pandemic – “masks are unnecessary”
In the early onset of the pandemic, nearly all organizations and specialists, including Dr. Anthony Fauci (March 8, 2020), advised against wearing a mask. The science simply did not support community wearing of masks:
“There’s no reason to be walking around with a mask,” infectious disease expert Dr. Anthony Fauci told 60 Minutes.
While masks may block some droplets, Fauci said, they do not provide the level of protection people think they do. Wearing a mask may also have unintended consequences: People who wear masks tend to touch their face more often to adjust them, which can spread germs from their hands.”[R]
Fauci later walked back those comments and tried to explain his comments were taken out of context. Instead of saying he was wrong and pointing to scientific evidence that caused him to change his mind, he obfuscated.
Here’s an infographic made by the World Health Organization (WHO) in late 2019.
“For healthy people, wear a mask only if you are taking care of a person with suspected 2019-nCoV infection”
There is no better example of the lack of scientific clarity on community mask wearing than the CDC’s flip-flopping on the issue. Initially, the CDC recommended against community mask wear, then reversed that position a few weeks later.
The CDC and WHO appear to be in disagreement on this recommendation. CDC (currently) recommends community mask wear, whereas the WHO does not…and they confirmed this fact again on March 31, 2020:
Canada Officially Recommends Against Community Wearing of Masks
On the official website of the Canadian government, a page lists many reasons why homemade masks are practically useless while also hindering oxygen intake.
Homemade masks are not medical devices and are not regulated like medical masks and respirators. Their use poses a number of limitations:
- they have not been tested to recognized standards
- the fabrics are not the same as used in surgical masks or respirators
- the edges are not designed to form a seal around the nose and mouth
- they may not provide complete protection against virus-sized particles
- they can be difficult to breathe through and can prevent you from getting the required amount of oxygen needed by your body
These types of masks may not be effective in blocking virus particles that may be transmitted by coughing, sneezing or certain medical procedures. They do not provide complete protection from virus particles because of a potential loose fit and the materials used.
Regardless, the debate rages on the internet and in the public spaces everywhere regarding whether or not to wear a surgical mask.
CDC supports homemade cloth masks…but the science does not
Cloth masks have no place in disease mitigation. They have been shown to be ineffective and worse (see below).
The CDC currently recommends (and some states mandate[R][R]) that everyone wear some form of face cover anytime they leave their home and enter the public space.[R] The CDC admits compliments but does not replace the President’s Coronavirus Guidelines for America, 30 Days to Slow the Spread.[R]
(None of the studies referenced by the CDC represent clinical research on the public use of face masks.[R])
The CDC even provides detailed instructions for how you can make your own face covers from common household items.[R]
I have no idea where the CDC and state public health advisors obtain their science, but apparently it is not the medical literature.
Cloth masks: Dangerous to your health?
It should be well known that cloth masks, bandannas, or handkerchiefs will do very little to stop the spread of coronavirus. The penetration of cloth masks by particles was almost 97% compared to medical masks with 44%.[R][R] In fact, they may actually increase your risk of becoming ill from CoVID-19 and other influenza-like illnesses.
One study that evaluated the use of cloth masks in a healthcare facility found that health care workers using cotton cloth masks were at increased risk of infection compared with those who wore medical masks. The authors concluded, “Cloth masks should not be used by workers in any healthcare setting.”[R][R]
Another reason not to wear a cloth mask. It could burn your face, eyes, and lungs.
Tennessee bought 5 million cloth masks[R] treated with DuPont’s Silvadur, an EPA listed hazardous pesticide.[R]
Public health agencies made recommendations but failed to provide guidance on proper handling and wear
The public is untrained in the sterile techniques required to make medical mask wear effective. Medical masks, worn and handled improperly, will not protect the wearer or those with whom they come in contact, instead, they will increase the spread of disease. The public health agencies and experts failed to anticipate how the public might not understand the principles of sterility essential to proper mask wear. And they failed to provide adequate resources, guidance, and instruction to the public.
After seeing the public mis-wearing and mis-handling masks in the real world, it is absolutely clear how misguided and dangerous this recommendation was from the CDC.
I have watched as people continuously touch and fidget with their masks. I watch them pull them down from their mouths and noses and rest it on their chin or neck. In doing so they contaminate the mask and themselves and then increase the spread of disease. The public simply has no idea how to safely cover their faces or wear gloves in a way that might slow the spread of disease.
Medical masks must be properly fitted and sealed around the mouth and nose. Masks must not be touched. Every touch has the potential to contaminate the mask and the hands, thus increasing the spread of disease.
Medical masks are single use devices designed to be worn for a relatively short period of time. Once the mask becomes saturated with moisture from breath, which, if properly fit, takes about an hour, they should be replaced. The more moisture-saturated the mask becomes, the more it blocks oxygen, increases re-breathing of carbon dioxide, re-breathing of viral particles, and becomes a breeding ground for other pathogens.
The longer masks are worn, the more they are touched, and the more contaminated they become. In addition to capturing pathogens on their outer surface, masks also quickly become moist, warm breeding grounds for bacteria and fungi. Thus, these opportunistic pathogens increase the risk of disease as they are inhaled into the airways, transferred to the hands, and end up on anything touched.
Unless medical masks are worn and handled properly, with strict adherence to sterility practices, medical masks worn by the community are prescriptions for disease and disaster.
What the CDC and WHO should have said about when and how to wear medical masks
- If you are healthy, you only need to wear a mask if you are taking care of a person with COVID-19.
- Wear a mask if you are infected with CoVID-19 or another infectious disease.
- Wear a mask if you are coughing or sneezing. Better yet, STAY HOME.
- If you wear a mask, then you must know how to use it and dispose of it properly.
- Mask type matters
-
- Medical grade surgical masks should be handled properly, never touched, and never reused
- Medical grade N95 masks/respirators work best
- Cloth masks, bandannas, scarves, and homemade masks are useless and potentially worse than not wearing a mask
Rigorous sterility maintenance techniques required
- Masks are effective only when used in combination with frequent washing with soap and water and strict sterility management techniques.
- Before putting on a mask, clean hands with soap and water. Only use alcohol-based hand cleaners when soap and water are not available.
- Cover your mouth and nose with the mask and make sure there are no gaps between your face and the mask. Proper wear, fit, handling, and disposal are critical to efficacy.
- Avoid touching the mask while using it; if you do, clean your hands with alcohol-based hand rub or soap and water.
- Replace the mask with a new one as soon as it is damp and do not reuse single-use masks.
- To remove the mask: remove it from behind (do not touch the front of the mask); discard immediately in a closed bin; clean hands with alcohol-based hand rub or soap and water.
- No mask should be worn and reused (unless it is properly sterilized, which is highly unlikely to occur in the general public)
Experts Speak Out
If you don’t believe me, listen to what these experts have to say:
Dr. Brosseau, a national expert on respiratory protection and infectious diseases
In April, Dr. Brosseau, a national expert on respiratory protection and infectious diseases at the University of Illinois at Chicago published an article titled “Masks-for-all for COVID-19 not based on sound data”. She wrote:
“Sweeping mask recommendations—as many have proposed—will not reduce SARS-CoV-2 transmission, as evidenced by the widespread practice of wearing such masks in Hubei province, China, before and during its mass COVID-19 transmission experience earlier this year. Our review of relevant studies indicates that cloth masks will be ineffective at preventing SARS-CoV-2 transmission, whether worn as source control or as PPE.
Surgical masks likely have some utility as source control (meaning the wearer limits virus dispersal to another person) from a symptomatic patient in a healthcare setting to stop the spread of large cough particles and limit the lateral dispersion of cough particles. They may also have very limited utility as source control or PPE in households.
If masks had been the solution in Asia, shouldn’t they have stopped the pandemic before it spread elsewhere?”
Top immunologist, Prof. Dolores Cahill
Top immunologist, Prof. Dolores Cahill, who has studied coronaviruses for years explains: once you’ve had the novel Coronavirus, you are immune; masks & social distancing do not affect coronavirus transmission; and how this lockdown was a mistake. Watch the full Dr. Dolores Cahill interview on the Highwire with Del Bigtree
Covid-19: important potential side effects of wearing face masks that we should bear in mind
This is the letter Dr. Cahill wrote to the British Medical Journal:
In their editorial to the BMJ,[1] Greenhalgh et al. advise that surgical masks should be worn in public to prevent some transmission of covid-19, adding that we should sometimes act without definitive evidence, just in case, according to the precautionary principle. The authors quote a definition of the precautionary principle found on Wikipedia, “a strategy for approaching issues of potential harm when extensive scientific knowledge on the matter is lacking.”
However, while no single formulation of that principle has been universally adopted,[2] the precautionary principle aims at preventing researchers and policy makers from neglecting potentially-harmful side effects of interventions. Before implementing clinical and public health interventions, one must actively hypothesize and describe potential side effects and only then decide whether they are worth being quantified or not.
Most scientific articles and guidelines in the context of the covid-19 pandemic highlight two potential side effects of wearing surgical face masks in the public, but we believe that there are other ones that are worth considering before any global public health policy is implemented involving billions of people.
The two potential side effects that have already been acknowledged are:
- Wearing a face mask may give a false sense of security and make people adopt a reduction in compliance with other infection control measures, including social distancing and hands washing.[3]
- Inappropriate use of face mask: people must not touch their masks, must change their single-use masks frequently or wash them regularly, dispose them correctly, and adopt other management measures, otherwise their risks and those of others may increase.[3,4]
Other potential side effects that we must consider are:
- The quality and volume of speech between two people wearing masks is considerably compromised, so they may unconsciously move closer. While one may be trained to counteract side effect n.1, this side effect may be more difficult to tackle.
- Wearing a face mask makes the exhaled air go into the eyes. This generates an uncomfortable feeling and an impulse to touch your eyes. If your hands are contaminated, you are infecting yourself.
- Face masks make breathing more difficult. For people with COPD, face masks are in fact intolerable to wear as they worsen their breathlessness.[5] Moreover, a fraction of carbon dioxide previously exhaled is inhaled at each respiratory cycle. Those two phenomena increase breathing frequency and deepness, and hence they increase the amount of inhaled and exhaled air. This may worsen the burden of covid-19 if infected people wearing masks spread more contaminated air. This may also worsen the clinical condition of infected people if the enhanced breathing pushes the viral load down into their lungs.
- The effects described at point 5 are amplified if face masks are heavily contaminated (see point 2)
- While impeding person-to-person transmission is key to limiting the outbreak, so far little importance has been given to the events taking place after a transmission has happened, when innate immunity plays a crucial role. The main purpose of the innate immune response is to immediately prevent the spread and movement of foreign pathogens throughout the body.[6] The innate immunity’s efficacy is highly dependent on the viral load. If face masks determine a humid habitat where the SARS-CoV-2 can remain active due to the water vapour continuously provided by breathing and captured by the mask fabric, they determine an increase in viral load and therefore they can cause a defeat of the innate immunity and an increase in infections. This phenomenon may also interact with and enhance previous points.
In conclusion, as opposed to Greenhalgh et al., we believe that the context of the current covid-19 pandemic is very different from that of the “parachutes for jumping out of aeroplanes”,[7] in which the dynamics of harm and prevention are easy to define and even to quantify without the need of research studies. It is necessary to quantify the complex interactions that may well be operating between positive and negative effects of wearing surgical masks at population level. It is not time to act without evidence.
Dr. Pamela Popper
Here’s what Dr. Pamela Popper said on her YouTube discussion of “What the Research Shows About Masks”
Masking the public was never about science…
Community wearing of face masks was never about science, health, or disease mitigation; it was always about symbolism, fear, and psychological operations to control the population.

Support your immune system!
https://meehanmd.ehealthpro.com/
Shop for high quality supplements recommended by Dr. Meehan at a discount.
Receive 15% OFF your first order:
USE PROMO CODE: FIRST15
Shipping is FREE on all orders and should arrive within 2-3 business days.
Read the full article at MeehanMD.com.
See Also:
New WHO Guidelines for Face Masks Admit No Known Medical Benefits – Psychological Brain Washing
References
Source: Health Impact News
Subscribe for natural health news to your inbox. Follow Natural Blaze on YouTube, Twitter and Facebook. Become a Patron for as little as $1 per month.