High-Risk HPV Type Replacement Follows HPV Vaccination
By James Lyons-Weiler, PhD
The number of studies that show that partial immunization via available HPV (human papillomavirus) vaccines is not only insufficient at reducing overall HPV infection rates; the vaccines actually cause rarer, more lethal types of HPV to sweep in and the net effect could be devastating increases in HPV-related cancers.
Here I review the biomedical research studies that show that type replacement is real, and that vaccination against the more common types may be, sadly and ironically, expected to cause INCREASES in HPV-related cancer.
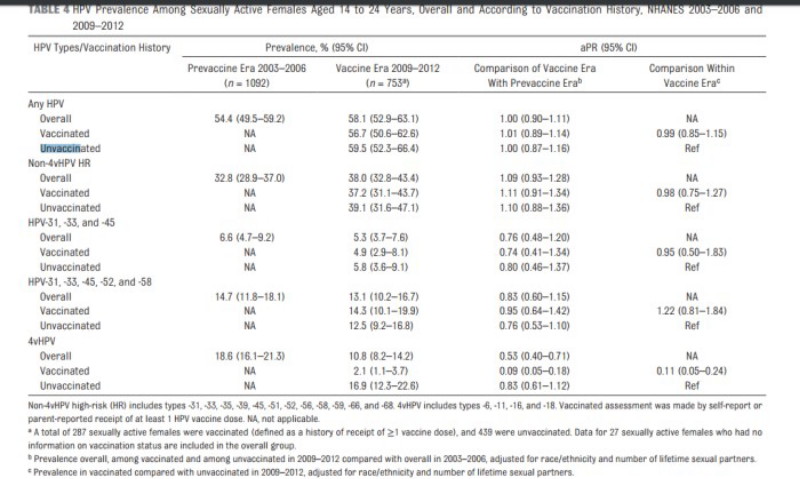
The first study is Center for Disease Control’s (CDC) own study, in which they show no net change in HPV infection rate (considering all types) after HPV vaccines were introduced into medical practice:
Markowitz LE et al., 2016 Prevalence of HPV After Introduction of the Vaccination Program in the United States. Pediatrics. 2016 Feb 22. pii: peds.2015-1968.
[do_widget id=text-16]
That study concluded that type replacement did not occur because their univariate analysis of individual types showed no individual type with a significant increase. However, because the vaccines do clear the vaccine-targeted types, the lack of change in overall infection rate shows that type replacement must be occurring.
The second study is by Fisher et al. (2016), which specifically found that high-risk HPV types replaced the vaccine-targeted types. They wrote “the percentage of non-vaccine HR-HPV types was higher than expected, considering that eight HPV types formerly classified as ‘low-risk’ or ‘probably high-risk’ are in fact HR-HPV types.”
Fischer et al 2016: Shift in prevalence of HPV types in cervical cytology specimens in the era of HPV vaccination. Oncol Lett. 12(1):601-610.
A third study is that by Guo et al., (2015) that also clearly found evidence of type replacement occurring as a result of HPV vaccination:
“The prevalence of high-risk nonvaccine types was higher among vaccinated women than unvaccinated women (52.1% vs 40.4%, prevalence ratio 1.29, 95% CI 1.06–1.57), but this difference was attenuated after adjusting for sexual behavior variables (adjusted prevalence ratio 1.19, 95% CI 0.99–1.43). HPV vaccination was effective against all 4 vaccine types in young women vaccinated after age 12. However, vaccinated women had a higher prevalence of high-risk nonvaccine types, suggesting that they may benefit from newer vaccines covering additional types.”
Guo et al., 2015. Comparison of HPV prevalence between HPV-vaccinated and non-vaccinated young adult women (20-26 years) American Association for Cancer Research Meeting, Apr 18-22; Philadelphia, PA. Philadelphia (PA): AACR; 2015. Abstract nr 844
A fourth study is that by Mollers et al., who wrote
“…our findings do suggest that clustering differs among HPV types and varies across risk groups.”
and
“The ecological niche could also be taken through type replacement, which refers to the possibility that elimination of HPV16 and HPV18 could lead to an increased transmission of nonvaccine types. For this to occur, antagonistic interactions are required between vaccine types and those not included in the vaccine (8, 9). Type replacement has been observed following vaccination against other pathogens (e.g., Streptococcus pneumoniae) (10) and is plausible whenever genotypically diverse pathogen strains compete for the same hosts.”
Mollers M et al., 2014. Population- and type-specific clustering of multiple HPV types across diverse risk populations in the Netherlands. Am J Epidemiol. 179(10):1236-46. doi: 10.1093/aje/kwu038.
A study of Italian women also considered type replacement and wrote that “an accurate post-vaccine surveillance is necessary to early detect a possible genotype replacement”:
Giambi C et al., 2013. A cross-sectional study to estimate high-risk human papillomavirus prevalence and type distribution in Italian women aged 18-26 years. BMC Infect Dis. 13:74. doi: 10.1186/1471-2334-13-74.
There are other studies that show type replacement. While some studies may show no type replacement, negative results do not take precedence over positive results. At best, one could say that the science is unsettled. However, CDC’s own study showed no net change in HPV infection rate, and studies now from the US, Germany, Italy and the Netherlands all support the same conclusions: there is evidence for grave concern over the adequacy of HPV vaccines: while the vaccine-targeted types are cleared, the hundred or so that can replace them across the sexually active population includes pathogenic types that may be more lethal than those targeted by the vaccines.
The statistics on the types that are said to be known to cause the most cancers are potentially misleading, because there is an inverse relationship between the ability of the pathogen to cause disease (morbidity) and death (mortality). If you count numbers of cases, yes, HPV-16 appears to be high-risk. But the low-frequency types may be even HIGHER risk – which would explain why they are low-frequency.
The study from Germany (Fisher et al., 2016) is definitive, and we have our answer: HPV type replacement is real, and is caused by partial vaccination against an oncogenic virus group.
Dr. James Lyons-Weiler, PhD is the author of several books, including “Ebola: An Evolving Story”, “Cures vs. Profits: Successes in Translational Research”, and “The Environmental and Genetic Causes of Autism”. He is the CEO and Director of IPAK, The Institute for Pure and Applied Knowledge, a not-for-profit pure public charity research institute focused on the reduction of human pain and suffering. You can support IPAK and its various projects, studies and initiatives at ipaknowledge.org. You can read more of Dr. Lyons-Weiler’s analyses at jameslyonsweiler.com and find his peer-reviewed publications at Pubmed.
Sign up for free news and updates from Robert F. Kennedy, Jr. and the World Mercury Project. Your donation will help to support us in our efforts.
This article appeared first at World Mercury Project and appears on Natural Blaze with permission.




