The FDA’s Disastrous War Against Sleep
 Authored by ‘A Midwestern Doctor’,
Authored by ‘A Midwestern Doctor’,
Story at-a-glance
- The power of sleep — Proper sleep is essential for our health, and disruptions can lead to severe issues like heart attacks, psychiatric illnesses, car accidents, fatigue, diabetes, cognitive impairment, and dementia.
- A widespread epidemic — Poor sleep affects many due to a lack of understanding about its importance and the use of sedative sleeping pills that hinder healthy sleep. For instance, medical training often deprives students of sleep, despite its critical role in learning.
- The forgotten miracle drug — In 1964, a remarkably effective sleeping medication hit the market, improving conditions like insomnia and overall health. However, its success threatened other drug markets. By 1990, the FDA and media launched a campaign against it, much like the case with ivermectin, resulting in the drug becoming almost unknown and many sleep disorders remaining untreated.
- What you’ll learn — This article delves into the harms of poor sleep, explores common causes, and uncovers effective treatments for sleeping disorders
One of the key themes I’ve tried to illustrate in my writings is that chronic illness has vastly increased over the last 150 years. A major cause of this is the disruption of the natural rhythms essential for our body’s self-regulation and self-repair.
Modern Medicine (Allopathy) often overlooks this concept because it doesn’t recognize the innate health of the body. Allopathic treatments focus on stabilizing or altering the body (e.g., ICU care or surgery) and hoping it heals itself, unlike other medical systems that enhance the body’s natural recovery capacity.
Typically, Allopathy excels with acute conditions, while a health-augmenting approach is better for chronic illnesses, an area where Allopathy often falls short. Here are three reasons why the Allopathic model dominates:
1. Economic incentives — The Allopathic model creates many expensive treatments and diagnostics, making it highly profitable and incentivizing its dominance in the medical market.
2. Cultural psychology — Our culture’s need to control and understand everything leads to methods that dominate nature rather than work harmoniously with it, oppose the philosophy of trusting the body’s natural healing.
3. Research bias — Medical research favors treatments that show immediate, observable changes (like lowering blood pressure) rather than those that promote gradual, long-term recovery, skewing the focus towards pharmaceutical interventions.
The Impact of Natural Rhythms on Health
The health of the body relies heavily on the normal functioning of self-regulating cycles:
• Breathing — Slow, smooth, nasal breathing profoundly impacts health and longevity by regulating many critical physiological functions.
• Sunlight — Regular exposure to sunlight is vital for health, and its absence doubles the risk of mortality and can lead to conditions like depression or cancer.
• Physical activity — Regular exercise is crucial, and a sedentary lifestyle leads to significant health issues. Those who walk daily often experience dramatically improved longevity.
• Mental rest — The mind needs to alternate between rest and activity, but modern life often forces constant thinking and stress.
In short, many of the natural rhythms our bodies rely upon for self-regulation are heavily disrupted in modern society, which in turn results in a variety of consistent derangements to normal physiology that are now seen throughout the population.
The Importance of Sleep
Throughout my career, I’ve met many integrative practitioners who emphasize normalizing their patient’s sleep as a crucial step in treating chronic illness. Sleep is a foundational process for restoring health, yet patients with chronic illnesses often suffer from disrupted sleep cycles, which can be challenging to correct.
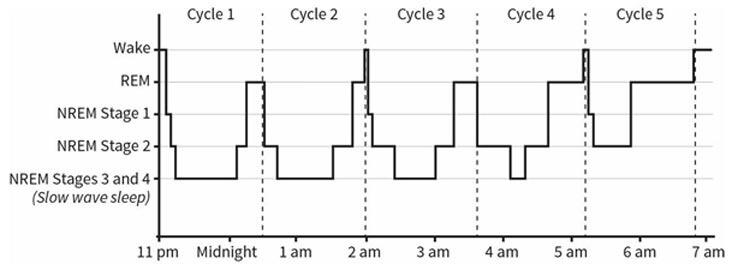
Sleep is a tightly regulated cycle, highly responsive to environmental signals and essential for maintaining other critical body rhythms. During sleep, the body cycles through different phases, each with critical functions: deep NREM sleep heals the brain and drains toxins, while REM sleep consolidates memories and processes emotions. A typical sleep cycle goes as follows:
Note: Since REM sleep predominates later at night, not sleeping long enough disproportionately disrupts REM sleep. NREM sleep is responsible for eliminating unnecessary memories, whereas REM sleep processes the day’s experiences and reinforces them into long-term memory.
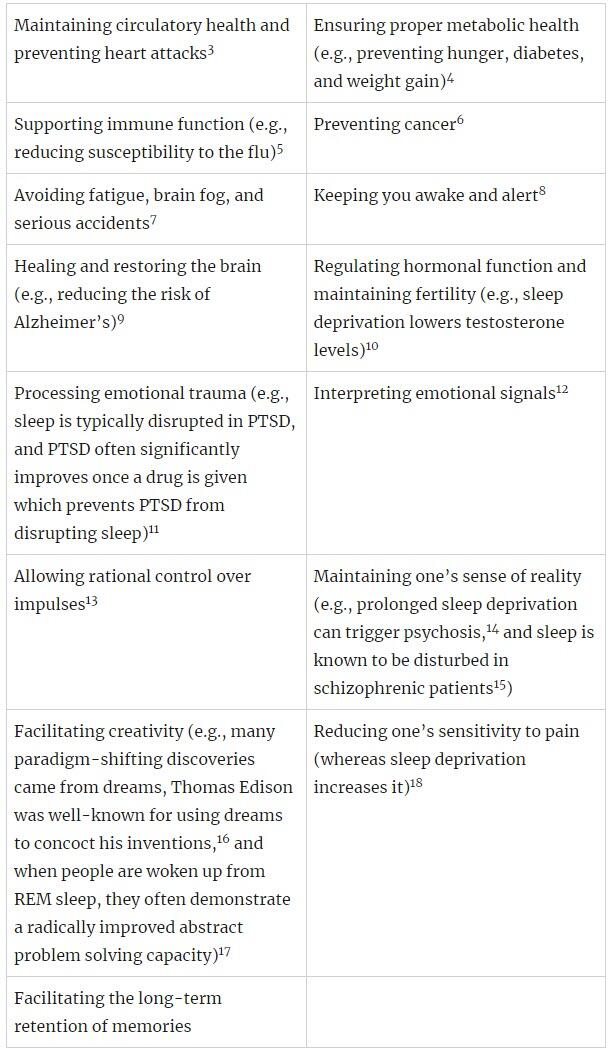
Matthew Walker is one of the world’s most vocal sleep researchers. In his book Why We Sleep, he argues that sleep serves several vital functions, including:
Any individual, no matter what age, will exhibit physical ailments, mental health instability, reduced alertness, and impaired memory if their sleep is chronically disrupted.
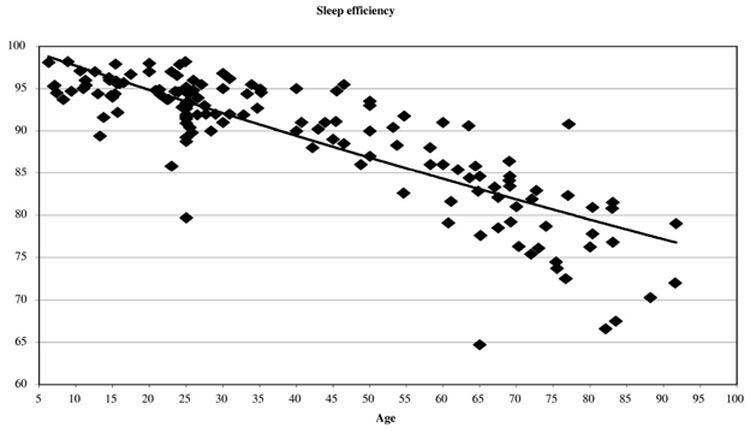
Even when controlling for factors such as body mass index, gender, race, history of smoking, frequency of exercise, and medications, the lower an older individual’s sleep efficiency score, the higher their mortality risk, the worse their physical health, the more likely they are to suffer from depression, the less energy they report, and the lower their cognitive function, typified by forgetfulness.
The Sleep Crisis
Adequate sleep requires:
- Sufficient time set aside for sleep.
- Ability to fall asleep quickly.
- Cycling through all sleep phases once asleep.
Adults generally need 7 to 9 hours per night, with infants and children needing more. Unfortunately, many people don’t get enough sleep, contributing to widespread health issues.
Key points:
- Gallup poll 57% of Americans want more sleep; only 42% get enough.
- 35.5% of American adults sleep less 7 hours per night; 30% have insomnia symptoms.
- 13.5% of adults feel tired most days; 10 days of 6-hour deficient sleep is equivalent to 24 hours of being awake (no sleep).
- Sleep Apnea affects 9% to 38% of the population.
- 30% to 48% of the elderly have insomnia symptoms, and 12% to 20% have insomnia disorders. Aging reduces sleep efficiency and quality and increases nighttime awakenings.
Sleeping Pills
Despite a $65 billion annual market for sleep aids in the U.S.24 and a $432 billion global “sleep economy” 50 to 70 million Americans suffer from sleep disorders. The pandemic worsened sleep for over half of Americans in 2020, and 76% admitted to buying sleep aids.
The problem lies in the nature of most sleeping pills: they are sedatives, not sleep aids. They sedate the brain, impairing its ability to initiate restorative sleep, leaving users tired and at risk for health issues.
Studies have shown that sleeping pill users are significantly more likely to die early and develop cancer. For example, one study found a twofold increase in mortality for sleeping pill users, with another study reporting a 3.6 to 5.4 times higher death rate for users over 2.5 years, and an increased cancer risk of 7% to 99%.
This in turn, led the authors to conclude that in 2010, prescription sleeping pills “may have been associated with 320,000 to 507,000 excess deaths within the USA alone.”
Most prescription sleeping pills, like Ambien, are “sedative hypnotics” similar to benzodiazepines (e.g., Valium), which are addictive and often used long-term despite being intended for short-term use. Over-the-counter options, like Benadryl or Unisom, are antihistamines that also disrupt the sleep cycle. Alcohol, with a similar mechanism to benzodiazepines, is another addictive sedative that inhibits sleep long after being ingested.
Gamma-Hydroxybutyrate
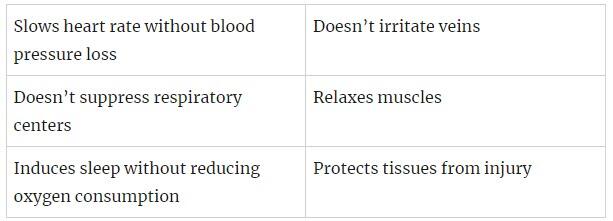
While most sleeping medications are unsafe and ineffective, one drug, gamma-hydroxybutyrate (GHB), has shown remarkable results. Developed in 1874, GHB was marketed in Europe as an intravenous anesthetic in 1964. Despite its benefits, it wasn’t practical for surgeries but was useful in intensive care due to its unique properties:
Decades of research followed and demonstrated GHB’s extraordinary properties and low toxicity. It metabolizes to succinate and water, has a high LD50, and no deaths have been conclusively attributed to it. GHB is a powerful sleep aid, restoring deep sleep cycles and leaving individuals refreshed — in many cases after just 3 to 4 hours of sleep.
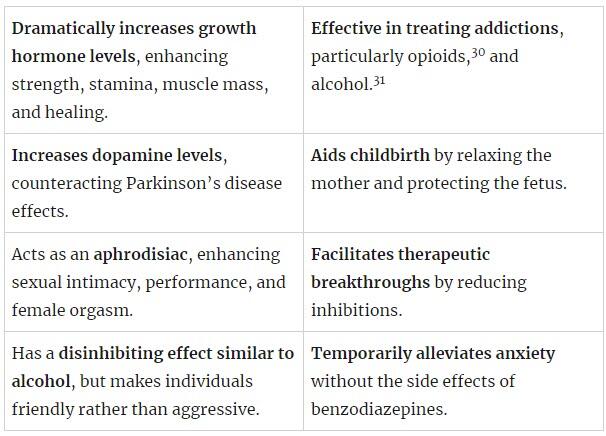
As more scientists (and then members of the public) began exploring the drug, according to Ward Dean MD29 (who provided extensive references to support his claims), through decades of research, they found a variety of benefits from GHB including:
Given these remarkable benefits and the decades of research supporting its use, why has no one ever heard of it?
The Ivermectin of Sleep Medicines
The medical industry often uses public relations to create campaigns that generate profits at the expense of public health.
For instance, dermatologists rebranded themselves as skin cancer fighters, spreading hysteria about skin cancer and sunlight dangers. This transformed dermatology into a lucrative field, despite the essential health benefits of sunlight. Similarly, during COVID-19, the FDA downplayed the benefits of ivermectin and hydroxychloroquine, creating unwarranted fear and blocking their use.
GHB’s story mirrors this pattern. In the early 1990s, as it gained popularity as a supplement (largely due to bodybuilders recognizing the value of it increasing growth hormone in the body), the FDA and CDC publicized adverse reactions to it, despite no fatalities (e.g., hospital doctors misinterpreted the brief deep sleep it created as a coma requiring intubation).
As recounted by Ward Dean MD, this led to an FDA ban, highly deceptive press releases, and a variety of illegal enforcement actions that were eventually overturned in court.
The FDA then helped create a media hysteria over GHB, fueled by comparisons to Rohypnol (“Roofies”) and made up GHB tragedies, which led to its portrayal as a dangerous date-rape drug. This culminated in a 2000 Federal anti-date rape drug law 2000 that made GHB a Schedule I drug, while simultaneously enshrining a pharmaceutical GHB preparation as a Schedule III drug.
Note: To be a Schedule I drug, the substance cannot have an acceptable medical use, which is hence irreconcilable with the FDA-approved preparation of it being a Schedule III drug.
In reality, GHB was rarely involved in sexual assaults and had a distinct easily detectable taste. Misleading media reports and government actions overshadowed the actual data and research. Most remarkably GHB, Rohypnol (Roofies) avoided similar bans due to effective lobbying by its manufacturer, is still a schedule IV drug in America (where it was never brought to market), and remains legal in many countries. Here, Comedian Jimmy Dore covers the GHB saga in more detail:
The Aftermath
Because of this debacle, it became almost impossible to get GHB, and many leading integrative doctors at the time were disgusted with the FDA as they saw how much GHB benefitted their patients and treated a variety of immensely challenging illnesses.
Patients occasionally ask me for GHB, and I sadly have to explain the criminal penalties associated with Schedule I drugs. Ironically, while GHB was outlawed, the off-patent and easy to manufacture schedule III pharmaceutical preparation of it sodium oxybate38 (Xyrem), remained legal but is prohibitively expensive, costing between $60,000 to $100,000 annually, a figure desperate patients will pay for this live changing medication.
Despite evidence supporting GHB’s efficacy for conditions like alcohol addiction, fibromyalgia, and numerous debilitating sleep disorders,41 efforts to change the FDA’s perception of GHB as merely a date-rape drug have been unsuccessful.
At the same time, underground GHB use has persisted, both recreationally and amongst certain patient groups (e.g., veterans with PTSD) due to its unique effects (e.g., enhanced sensory experiences and sociability alongside its myriad of remarkable therapeutic benefits). Here, Joe Rogan and Jimmy Dore discuss where things currently stand with GHB:
Overall, one of the most extraordinary things about the GHB saga is that its many benefits discovered over the decades of research it received were then subsequently rediscovered by the sleep research community. This again illustrates how often the research we really need (and hence spend billions on each year) already exists but was simply buried due to it being inconvenient for the industry.
More than anything else, I believe the GHB story demonstrates the importance of not being overly biased. For example, while many doctors hold a strong prejudice against any “natural” (e.g., nondrug) therapy, I am the opposite and typically avoid using pharmaceutical drugs because of how frequently I find their harms outweigh their benefits.
Nonetheless, I periodically find extraordinary drugs I take a hard look at and end up using throughout my medical practice. Sadly, as the war against ivermectin showed the world, the primary motivation behind most of medicine is money, and as a result, whenever a highly beneficial drug is discovered that competes with existing drugs, the medical industry moves to bury it, regardless of how much evidence there is in support of it.
Note: The existing research on GHB is discussed in further detail here.
Sleep Hygiene
Let’s now look at other options for improving sleep. One of the most tried and true ones is to change the signals your body receives so it can go to sleep on its own. Here are key approaches:
1. Regulate circadian rhythm — The body’s natural cycle, governed by processes like adenosine buildup and circadian cues, signals when to sleep. Consistency in sleep and waking times is an essential piece of good sleep hygiene. Following environmental cues and natural cycles is ideal but often disrupted by modern lifestyles.
2. Address sleep barriers — Factors like age-related brain damage or fluid obstructions hinder sleep. Remedies such as electrically improving the body’s fluid circulation or reducing EMF exposure can help.
3. Avoid disruptive substances — Caffeine and alcohol, by blocking adenosine receptors or disrupting sleep cycles, impair sleep quality. Their effects linger due to varying metabolic rates, exacerbating sleep issues, especially as metabolism slows with age. One of the most intriguing data points I’ve seen about the effects of caffeine came from this NASA study.
4. Temperature management — Natural temperature drops aid sleep onset, making cooler environments conducive to rest. Techniques like cooling baths or sleeping in cooler rooms promote better sleep quality.
Note: One of the most interesting approaches to overcoming the temperature barrier for sleep was a study that found using a customized suit to externally drop people’s temperature made it much easier for them to sleep (especially in the elderly).
5. Manage light exposure — Blue light from screens disrupts melatonin secretion, crucial for sleep regulation. Using blue light filters, minimizing screen time before bed, and creating darker sleep environments support healthy sleep patterns.
6. Behavioral adjustments — Establishing bedrooms as sleep sanctuaries, maintaining consistent sleep-wake schedules, and practicing relaxation techniques before bed enhance sleep quality. Physical activity during the day and avoiding stimulating activities close to bedtime also aid in achieving restful sleep.
Note: Many people find cognitive behavioral therapy (CBT) to be extremely helpful for insomnia and there is now significant evidence to support it being a first-line therapy.
7. Diet and lifestyle — Maintaining a balanced diet, avoiding late-night eating, and monitoring caffeine intake play roles in promoting restorative sleep. Keeping a sleep journal can help identify triggers contributing to insomnia.
By addressing these facets, we can optimize sleep environments and routines, fostering healthier sleep patterns, without being dependent on the sleeping pill industry, and despite the absence of healthy therapeutic options (GHB) for more serious physiological ailments and sleep dysfunctions.
Conclusion
One of the things I’ve repeatedly heard people say through COVID-19 was “if they did this with ivermectin (or hydroxychloroquine), what else have they done this with?” Here, I provide one such example, and sadly, the GHB story is by no means an isolated example (e.g., others are discussed here).
However, while the GHB story is atrocious, on one level I am grateful for it, as had a safe and effective cure for insomnia existed, we likely would have never been forced to learn what the actual underlying causes of sleep impairment are, and likewise, our society would have never conducted the research which demonstrated just how critically important sleep is.
Sadly, one of the greatest problems in medicine is that it typically takes 17 years for scientific discoveries to change the practice of medicine. In turn, despite the dire need for improved sleep in society, it is unlikely this problem will be addressed by the mainstream for a long time (even in areas like intellectually based professions or education where the cognitive impairment resulting from poor sleep is highly counterproductive to the goals of the institution).
I hope the knowledge provided here has given you an appreciation for the importance of healthy sleep and a few helpful approaches you can incorporate into your life!
Author’s note: This is an abbreviated version of a full-length article that takes a deeper look into the causes and treatments of insomnia. For the entire read with much more specific details and sources, please click here.
Sourced from ZeroHedge